Protein C deficiency
| Protein C deficiency | |
|---|---|
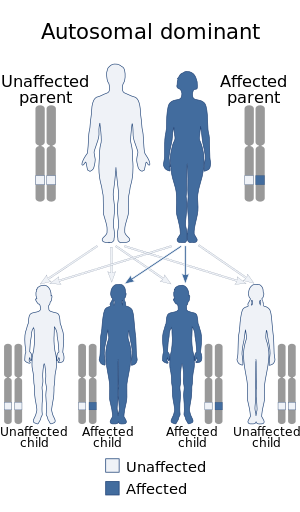 | |
| This condition is inherited in an autosomal dominant manner | |
| Specialty | Hematology |
Protein C deficiency is a rare genetic trait that predisposes to thrombotic disease. It was first described in 1981.[1] The disease belongs to a group of genetic disorders known as thrombophilias. Protein C deficiency is associated with an increased incidence of venous thromboembolism (relative risk 8–10), whereas no association with arterial thrombotic disease has been found.[2]
Contents
1 Presentation
1.1 Complications
2 Pathophysiology
3 Diagnostic testing
4 Treatment
5 Epidemiology
6 References
7 External links
Presentation
Complications
Protein C is vitamin K-dependent. Patients with Protein C deficiency are at an increased risk of developing skin necrosis while on warfarin. Protein C has a short half life (8 hour) compared with other vitamin K-dependent factors and therefore is rapidly depleted with warfarin initiation, resulting in a transient hypercoagulable state.
Pathophysiology
The main function of protein C is its anticoagulant property as an inhibitor of coagulation factors V and VIII. A deficiency results in a loss of the normal cleaving of Factors Va and VIIIa. There are two main types of protein C mutations that lead to protein C deficiency:[2]
Type I: Quantitative defects of protein C (low production or short protein half life)
Type II: Qualitative defects, in which interaction with other molecules is abnormal. Defects in interaction with thrombomodulin, phospholipids, factors V/VIII and others have been described.
The majority of people with protein C deficiency lack only one copy of the functioning genes, and are therefore heterozygous. Before 1999, only sixteen cases of homozygous protein C deficiency had been described (two abnormal copies of the gene, leading to absence of functioning protein C in the bloodstream). This may manifest itself as purpura fulminans in newborn babies.[2]
Diagnostic testing
There are two main types of protein C assays, activity and antigen (immunoassays).[3] Commercially available activity assays are based on chromogenic assays that use activation by snake venom in an activating reagent, or clotting and enzyme-linked immunosorbant assays.[4] Repeated testing for protein C functional activity allows differentiation between transient and congenital deficiency of protein C.[3][5]
Initially, a protein C activity (functional) assay can be performed, and if the result is low, a protein C antigen assay can be considered to determine the deficiency subtype (Type I or Type II). In type I deficiencies, normally functioning protein C molecules are made in reduced quantity. In type II deficiencies normal amounts of dysfunctional protein C are synthesized.[3]
Antigen assays are immunoassays designed to measure the quantity of protein C regardless of its function. Type I deficiencies are therefore characterized by a decrease in both activity and antigen protein C assays whereas type II deficiencies exhibit normal protein C antigen levels with decreased activity levels.[3]
The human protein C gene (PROC) comprises 9 exons, and protein C deficiency has been linked to over 160 mutations to date.[6][7] Therefore, DNA testing for protein C deficiency is generally not available outside of specialized research laboratories.[3]
Manifestation of purpura fulminans as it is usually associated with reduced protein C plasma concentrations of <5 mg IU/dL.[5] The normal concentration of plasma protein C is 70 nM (4 µg/mL) with a half live of approximately 8 hours.[1] Healthy term neonates, however, have lower (and more variable) physiological levels of protein C (ranging between 15-55 IU/dL) than older children or adults, and these concentrations progressively increase throughout the first 6 months of life.[8] Protein C levels may be <10 IU/dL in preterm or twin neonates or those with respiratory distress without manifesting either purpura fulminans or disseminated intravascular coagulation.[9]
Treatment
Primary prophylaxis with low-molecular weight heparin, heparin, or warfarin is often considered in known familial cases. Anticoagulant prophylaxis is given to all who develop a venous clot regardless of underlying cause.[4]
Studies have demonstrated an increased risk of recurrent venous thromboembolic events in patients with protein C deficiency. Therefore, long-term anticoagulation therapy with warfarin may be considered in these patients.[4]
Homozygous protein C defect constitutes a potentially life-threatening disease, and warrants the use of supplemental protein C concentrates.[10]
Liver transplant may be considered curative for homozygous protein C deficiency.[10]
Epidemiology
Heterozygous protein C deficiency occurs in 0.14–0.50% of the general population.[11][12] Based on an estimated carrier rate of 0.2%, a homozygous or compound heterozygous protein C deficiency incidence of 1 per 4 million births could be predicted, although far fewer living patients have been identified.[4] This low prevalence of patients with severe genetic protein C deficiency may be explained by excessive fetal demise, early postnatal deaths before diagnosis, heterogeneity in the cause of low concentrations of protein C among healthy individuals and under-reporting.[4]
The incidence of protein C deficiency in individuals who present with clinical symptoms has been reported to be estimated at 1 in 20,000.[13]
References
^ ab Griffin JH, Evatt B, Zimmerman TS, Kleiss AJ, Wideman C (1981). "Deficiency of protein C in congenital thrombotic disease". J. Clin. Invest. 68 (5): 1370–3. doi:10.1172/JCI110385. PMC 370934. PMID 6895379..mw-parser-output cite.citation{font-style:inherit}.mw-parser-output .citation q{quotes:"""""""'""'"}.mw-parser-output .citation .cs1-lock-free a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .citation .cs1-lock-limited a,.mw-parser-output .citation .cs1-lock-registration a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .citation .cs1-lock-subscription a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration{color:#555}.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration span{border-bottom:1px dotted;cursor:help}.mw-parser-output .cs1-ws-icon a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/4/4c/Wikisource-logo.svg/12px-Wikisource-logo.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output code.cs1-code{color:inherit;background:inherit;border:inherit;padding:inherit}.mw-parser-output .cs1-hidden-error{display:none;font-size:100%}.mw-parser-output .cs1-visible-error{font-size:100%}.mw-parser-output .cs1-maint{display:none;color:#33aa33;margin-left:0.3em}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-format{font-size:95%}.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-left{padding-left:0.2em}.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-right{padding-right:0.2em}
^ abc Khan S, Dickerman JD (2006). "Hereditary thrombophilia". Thromb J. 4 (1): 15. doi:10.1186/1477-9560-4-15. PMC 1592479. PMID 16968541.
^ abcde Khor B, Van Cott EM (2010). "Laboratory tests for protein C deficiency". Am J Hematol. 85 (6): 440–442. doi:10.1002/ajh.21679. PMID 20309856.
^ abcde Goldenberg NA, Manco-Johnson MJ (2008). "Protein C deficiency". Haemophilia. 14 (6): 1214–1221. doi:10.1111/j.1365-2516.2008.01838.x. PMID 19141162.
^ ab Chalmers E, Cooper P, Forman K, Grimley C, Khair K, Minford A, Morgan M, Mumford AD (2011). "Purpura fulminans: recognition, diagnosis and management". Arch Dis Child. 96 (11): 1066–1071. doi:10.1136/adc.2010.199919. PMID 21233082.
^ D'Ursi P, Marino F, Caprera A, Milanesi L, Faioni EM, Rovida E (2007). "ProCMD: a database and 3D web resource for protein C mutants". BMC Bioinformatics. 8 (Suppl 1): S11. doi:10.1186/1471-2105-8-s1-s11. PMC 1885840. PMID 17430555.
^ Rovida E, Merati G, D'Ursi P, Zanardelli S, Marino F, Fontana G, Castaman G, Faioni EM (2007). "Identification and computationally-based structural interpretation of naturally occurring variants of human protein C". Hum Mutat. 28 (4): 345–55. doi:10.1002/humu.20445. PMID 17152060.
^ Williams MD, Chalmers EA, Gibson BE (202). "The investigation and management of neonatal haemostasis and thrombosis". Br J Haematol. 119 (2): 295–309. doi:10.1046/j.1365-2141.2002.03674.x. PMID 12406062.
^ Manco-Johnson MJ, Abshire TC, Jacobson LJ, Marlar RA (1991). "Severe neonatal protein C deficiency: prevalence and thrombotic risk". J Pediatr. 119 (5): 793–798. doi:10.1016/s0022-3476(05)80305-1. PMID 1834822.
^ ab Kroiss S, Albisetti M (2010). "Use of human protein C concentrates in the treatment of patients with severe congenital protein C deficiency". Biologics. 4 (5): 51–60. doi:10.2147/btt.s3014. PMC 2846144. PMID 20376174.
^ Miletich J; Sherman L; Broze G, Jr (1987). "Absence of thrombosis in subjects with heterozygous protein C deficiency". N Engl J Med. 317 (16): 991–996. doi:10.1056/NEJM198710153171604. PMID 3657866.
^ Tait RC, Walker ID, Reitsma PH, Islam SI, McCall F, Poort SR, Conkie JA, Bertina RM (1995). "Prevalence of protein C deficiency in the healthy population". Thromb Haemost. 73 (1): 87–93. PMID 7740502.
^ Dahlback B. (1995). "The protein C anticoagulant system: inherited defects as basis for venous thrombosis". Thromb Res. 77 (1): 1–43. doi:10.1016/0049-3848(94)00138-4. PMID 7701473.
External links
| Classification | D
|
|---|---|
| External resources |
|